by phoebescopes | Jul 25, 2020 | Thoughts on Health
Our brains are described a being plastic. They continually remould neural connections as we learn experience and adapt.
When I was a child, I would sometimes imagine being small enough to get into a bubble that would take me on a journey around the inside of the body.
I had it all worked out…Skin was represented by a large blanket that I used to covered my tree house with.
Blood was the river that my bubble was floating on; that took me through the body…and bones were mountains, caves and crevices on the adventure.
Looking back on my imagination and my floating bubble, I realize that at that time in my life, I was just curious about finding the places in my body that were not well, so that they could be repaired.
You see, I spent periods of my childhood in hospital, undergoing surgery for a spine problem I had. It was either that or I was attending appointments with the specialists or having physiotherapy.
Throughout this time, I felt that whatever I was suffering from could be fixed.
Of course now as an adult, I am a little more realistic about what can be achieved when dealing with life’s health challenges BUT I still believe that there is so much that we don’t know about.
Maybe also being a survivor of meningitis and in a critical condition that doctors said I wouldn’t survive is a constant reminder of how unique we all are.
So, it’s safe to say that I’ve always been really fascinated with the complexities and magnificence of the human body and how it works.
If I hadn’t pursued my childhood passion that steered me towards the ‘Arts’, I feel sure that I would have taken a human biology path in the field of research for treatments to solve health problems.
Despite choosing the creative ‘Art’s field, I guess that my earliest life journey and experience with health issues has, in the background helped me develop as an avid researcher.
There are many subjects that interest me but none more than of that about the brain.
Over 20 years ago, I learned that scientists were now referring to the brain as being plastic.
This was a huge deal because before then, people did not believe that the brain could change or repair or be fixed if there was something wrong with it.
Scientists had believed that we were born with a certain number of non-replenishing cells that once used, or if damaged could not be repaired and would not be replaced. We now know that this is not true.
Correctly referred to as neuroplasticity, a study in 1998 found that the human brain has the ability to develop new brain cells and many studies followed, proving that the brain can change or be transformed to demonstrate plasticity.
A plastic brain!
I knew they didn’t mean it literally but at the time of hearing this news, I was briefly transported back to my child self again where I imagined everyone having a plastic brain.
I pictured the brain being made of multi-coloured building blocks that slotted together and I imagined that each block represented something that made us function.
Sadly, after accidents or as a result of various autoimmune diseases, many people are often still told that the damage sustained or created is permanent and this is clearly the case for many people.
Having said this, I don’t feel that this is in any way balanced with the fact that there are those that experience partial improvements when they were told this would never happen.
And, why is it that others can also even experience complete recovery of their disability over time?
Well, new connections can form, creating new pathways that ultimately change the structure of the brain. New neurons, also called nerve cells are constantly being born as old ones die but a balance of cells is maintained while the brain undergoes repair.
So you see, while I respect and appreciate the opinions of many medical professionals, they are not encouraged to spend too much time considering the unimaginable power that is always changing the brains potential.
For this reason, I remain completely in awe of the brain and what it is capable of achieving.
I have always referred to the brain as the hub, containing a network of muscles that support everything about us, so it’s easy to understand that some physical or mental difficulties can be downgraded or illuminated by exercising the associated brain muscles.
Below is a link to an interesting article
Repairing the brain
by phoebescopes | Jul 24, 2020 | Thoughts on Health
I was gripped with fear and terrified that I was going to drown and that my family would be the ones to find me in this state.
I imagined family members blaming themselves for not being there to save me, so I decided that I couldn’t go.
I closed my eyes and started breathing deeply and slowly and I began to visualise being able to move my left arm to reach the chain attached to the bath plug.
When I could eventually feel the chain, it took a while and every bit of focus to hook my finger around the chain, pulling the plug out from the plughole- allowing water to start draining away.
Listening to water draining away was emotionally overwhelming. I cried with joy but it wasn’t over yet…
I still hoped that the water would drain away quicker than the rate that I was still sliding under.
At last, I was lying in an empty bath tub-now cooling to the point that I felt quite cold and as my body temperature dropped, I was able to move my limbs and wiggle my fingers and toes again.
I lay in an empty bath, suffering from shock but thanking my spirit guide for keeping me company while I worked out my survival plan.
When I eventually got out of the bath and out of the bathroom, my husband couldn’t get a proper sentence out of me.
So what was actually happening during this time?
Known as: Heat Intolerance, Temperature or Heat sensitivity
There is a part of the brain called the hypothalamus which is responsible for controlling your body temperature, keeping it at the right temperature in hot or cold conditions. It does this by sending signals to the body to start sweating if it gets too hot, or shivering if it gets cold.
For those who have an existing medical condition, the hypothalamus does not work as well as it should and so may not be able to regulate the body so easily.
Many people enjoy warmer temperatures, but some people with autoimmune or neurological conditions such as; Hypothyroidism, Multiple Sclerosis, Fibromyalgia and Parkinson’s to name a few have problems in the heat.
Difficulties regulating body temperature can be a serious issue for this group of people because the heat can stop nerve fibres from working properly. This means that sometimes messages cannot get through to from the brain leaving sufferers to experience fatigue, weakness, difficulty breathing and problems with balance or vision.
These symptoms compromise safety and may create dangerous situations similar to the one I had.
But after almost a decade of avoiding the bath tub, I decided that with careful planning and now with a better understanding, I could return to having an occasional soak in the bath.
What are the things I do or use that make bath time safe again for me?
1 ) Use a rubber suction bath mats (reduces ability of slipping or sliding down in the bath tub
2 ) Position of plughole –
Ensure that the chain is securely connected to the plug and that you can usually reach this easily if required.
The plug hole being positioned in the middle of the tub instead of at the head or tail was a saving grace.
3 ) I keep a container of ice cold water next to me on the rim of the bath and drink this as soon as I begin to feel that I’m overheating.
4 ) On the very few occasions that I decide to have a soak in the bath, I don’t lock the door.
Thank you for reading my article
by phoebescopes | Jul 24, 2020 | Thoughts on Health
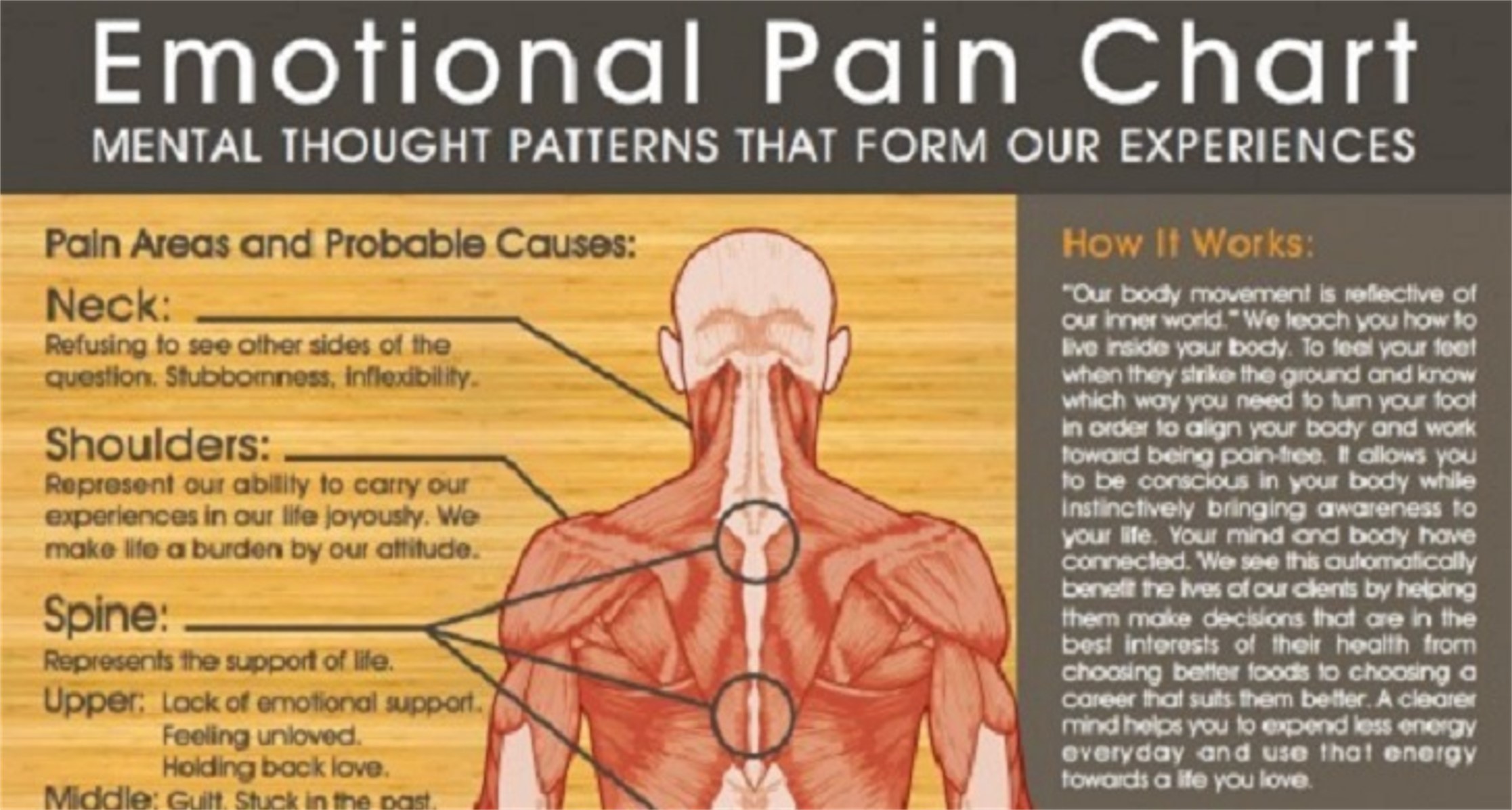
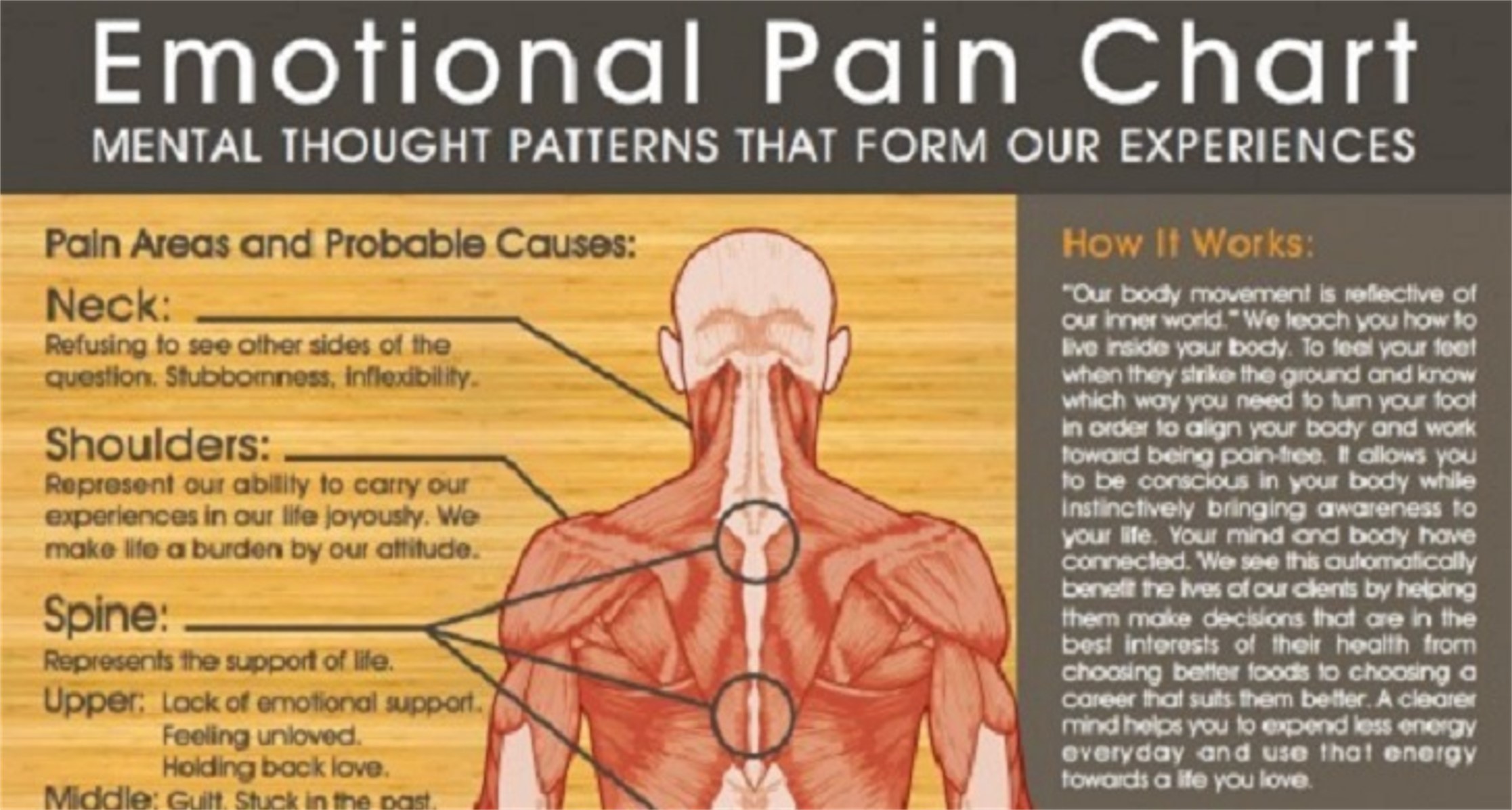
I was fortunate that for many previous years, I had remained unaffected by back problems or the acute back ache that I spent my childhood and teenage life living with, but for a number of reasons, some of the old, niggling pain had gradually resurfaced again.
Why was this happening now?
Well, I believe that this new wave of pain- slowly trying to take centre stage was actually triggered when I temporarily veered off my normal track from a natural and holistic practice in favour of receiving drug therapy for my autoimmune condition.
To begin with, it appeared that my decision was the right one to make because I experienced improvements to my condition but as months went by, I began to see a return of old symptoms and the start of new ones.
My body was reminding me of how sensitive it is to foreign, artificial and chemical substances.
I couldn’t really say I was surprised about the symptoms I experienced after using these medicines because this was actually the reason why I moved away from a drug based approach in favour of natural therapies.
It was definitely the case that I had forgotten how miserable and unwell I became when relying on a regular drug regime.
My immune system was struggling from a high toxic load that was creating more side effects as a result.
So, I accepted that I would again need to safeguard the condition of my immune system by minimising or illuminating the use of pharmaceuticals as much as possible.
So, what is the safest way to manage a symptom like pain?
Well, these days, I rarely turn to using pain killers to manage persistent pain because at best, they were sometimes effective in damping down pain but in place, left me with unwanted side effects; dry mouth, a bad sense of taste & smell, muscle cramp, skin irritations and irritable bowel (IBS).
Knowing that the risk- reward ratio of using pain medication weighed very heavy on the side of risk, and is detrimental to health has made my decision easier to make.
I decided to reserve medication such as painkillers for the times when I really need a full arsenal of pain busting relief. That score of 5 or more.
Why?
Well, because I believe that by turning to pain killers sparingly, I can increase their short term effectiveness, reduce or manage their unwanted side effects and greatly minimize any chance of building a dependency on them-needing higher doses; a dependency that would quickly render them ineffective so they no longer work in the future when I need them the most!
In all case, before I reach for pain killers, I follow a few steps to assess how bad pain really is.
I work on a scale in my head…a scale of 1 to 5 – where 1 is my normal (a little pain) and 5 is unmanageable. I acknowledge the pain I’m experiencing and try to work out why it is there and then I start building a plan of action to ease things.
I notice that however much pain I’m experiencing, the first thing I find helpful to do is to move around instead of trying to avoid the problem areas. I touch, massage, stretch and connect with my painful site.
Although this can often be uncomfortable, I remember how important it is to ensure the movement of blood and oxygen to damaged areas to prevent premature cell death and permanent damage while promoting repair.
The plan also usually calls for me to ‘up’ my physical activity, so I make an extra point of walking around my home-using the stairs- pausing on each step to stretch out my limbs. Stair rails, ledges, shelving, chairs and tables become even more useful as makeshift exercise equipment!
I also begin to focus on and look forward to a swimming session and imagine the weightlessness and freedom I feel as I move through the water.
It’s amazing how focusing on these strategies has a subtle ability of downgrading the initial pain and discomfort I started with and developing this process is an effective distraction strategy that works to put my body, mind & soul into a relaxed space-ready to begin the process of healing.

by phoebescopes | Jul 23, 2020 | Thoughts on Health
There is no questioning the fact that we are living in a time where so much amazing technology has been created and is being used to detect medical problems, fix health issues and save lives.
Having survived a medical scare as a baby, I know that without the equipment used at that time, I would likely not be here today but with all of this technology telling us what’s right or wrong with us, are we seeing a new kind of problem that technology can’t help us with?
Do we rely too much on what technology tells us instead of what our body is telling us?
My focus and questions are aimed at the work of an MRI machine (Magnetic Resonance Imaging). A scanning procedure first used in 1977 to diagnose cancer and now used to detect many other problems or determine the severity of certain injuries.
An MRI machine uses a magnetic field and radio waves to create detailed images of the body, so it also has the ability to detect inflammation.
For a condition like mine (Multiple Sclerosis), MRI is routinely used to determine whether there is active inflammation in the brain and/or spinal cord.
So, why is it useful to be able to detect certain kinds of inflammation?
Inflammation is a process by which the body’s white blood cells and substances they produce protect us from infection with foreign organisms, such as bacteria and viruses.
Inflammation is a natural AND necessary occurrence in our body.
However, in some diseases like Multiple Sclerosis for example, the body’s defence system (the immune system) falsely triggers an inflammatory response when there are no foreign invaders to fight off.
Here, the body responds as if normal tissues are infected or somehow abnormal and begins to attack them, believing that they hold bacteria or virus when in reality these tissues have nothing wrong with them.
These false triggers are common in what are known as autoimmune diseases like multiple sclerosis, rheumatoid arthritis and Parkinson’s and they often lead to mental and/or physical impairment as a result of damage to the body’s own tissues.
Many neurologists use MRI as the Holy Grail to decide the course of treatment for patients like me. They often favour treating patients that clearly show signs of some sort of inflammatory activity, seen by MRI.
Doctors believe that, seeing inflammation (an attack of the tissues) as it takes place provides clear evidence and offers better treatment results.
This way of utilizing MRI often means that without a clear sign of inflammation, patients are not considered for treatments that could actually improve their quality of life.
Although I experienced intermittent periods of visual disturbance, problems with balance or sensory discomfort (pain in my leg), I remained completely active. So in the early days after being diagnosed with Multiple Sclerosis, my life was quite unchanged.
An MRI carried out at this time did not indicate inflammation but did show lesions (scarring) which was indication of an inflammatory response in the war that had previously taken place in my brain.
In my case, the MRI results didn’t match up with the symptoms I was having or how I was feeling and without any signs of active inflammation, I was not considered a good candidate to receive treatment that had a 75% chance of stopping my disease from progressing further.
Fighting another kind of war
If it wasn’t enough that I had an inflammatory war going on inside me that MRI could not accurately detect, I now had to fight a political war against medical authorities who felt strongly that treatment would be ineffective without signs of inflammation.
I was by then beginning to experience an increase in symptoms and gradually became aware that I could no longer do certain things with ease. The results of my MRI might not have shown inflammation but it was clear that my immune system was under siege!
My compromised immune system now showed evidence of damage in the shape of mild physical impairment and I decided that I would need to act fast to try and prevent further loss occurring.
So, with no likely treatment option available for me at home, I cast my research net out wider and visited a hospital facility abroad that were successfully using a treatment protocol I wished to have.
In this highly experienced facility, thousands of miles away from home, I again had to go through a battery of tests including receiving another MRI.
Results were the same. “No active inflammation” and my heart sank with this news but the doctor did not stop at the results of an MRI. He assessed me further, taking into account other key factors about me such as- my age, medical history, attitude to potential risks and essentially how I was feeling at this time.
After 10 days of tests, the doctor was satisfied with my results and treatment was commenced.
Despite not having active inflammation on the results of my MRI both at home and abroad, I was amazed when I began to experience cognitive improvements soon after completing the treatment regime.
For me, this was a powerful indication that there had been some underlying inflammatory activity not previously picked up by MRI.
According to various articles I had read and the belief of many doctors, this treatment didn’t work and was deemed as very dangerous.
I was not supposed to benefit from having this therapy but I did and I am so grateful to have met an amazing doctor-thousands of miles away from home that treated me as an individual and wanted to help.
So, my brain has remained clear and fog free for over 6 years. My memory is sharp, I no longer slur my words as though drunk or lose the frame of sentences and 12 months post treatment, I was able to start designing again.
In fact, just producing this article speaks volumes about some of the improvements I experienced because many would not have been possible without taking a well researched and calculated but still big risk to try improve my quality of life.
My restricted mobility remains a working progress and is a reminder of what the wrong kind of inflammation can do to the body.
Although my life is different now, I am hugely grateful to have a productive quality of life that continues to improve instead of deteriorate.
I still believe in the power of MRI for its ability to investigate and pin point all kinds of medical problems including detecting inflammation at the earliest possible time of disease. While this provides both doctor and patient with more time and maybe more choices of how to manage conditions and disease, I see and have experienced the power of physiology.
Looking back on my experience, I definitely felt blessed to be given the opportunity to step out of my disease- becoming more conscious of the things that were contributing to my condition and learning how to avoid certain triggers.

by phoebescopes | Jul 23, 2020 | Thoughts on Health
I was 9 years old and was having emergency major surgery to fuse vertebra in my spine.
I could see myself lying, shrouded on the operating table and there were other people in the room. Some of them were standing over me.I could hear music and a low, softly spoken voice of authority. The voice sounded like a man’s voice and I remember thinking that he sounded like Mr Kelly, my head teacher at school.
I drifted away from that thought and tuned in to the faint sound of some music I could here on a radio but I couldn’t quite make out what was playing.
It didn’t seem to matter that I couldn’t identify the music anyway because an inner thought had already moved me on to create a rhythm that merged this music with the bleeps from monitors in the room. I was enjoying this game. It was fun!
I felt no pain; just an excitement that maybe I was being abit naughty-getting away with eavesdropping on BIG PEOPLE’S conversation because I could see and hear them but was sure they had no idea of this.
So, there I lay… feeling completely relaxed but suddenly, the music was being drowned out by loud voices and noises and I started flying around the room to try and get a better view of what was happening to me.
I was on the operating table but I was no longer responsive. The bleeps were replaced with the sound of a continuous hum. They made a number of attempts to revive me but I was lost.
Shortly after this, a member of the medical team informed my mother that there had been complications but somehow, somewhere, ‘I’ was not done yet. A faint pulse had been pushing its way through and had left doctors perplexed but this was enough to have me rushed off to the intensive care unit for emergency observation without a moment to spare. I remained there in a critical condition for a number of days.
I learnt that I suffered a massive, life threatening reaction to a drug I was given during the operation and had quickly developed a condition called Malignant Hyperpyrexia.
Later in life, during a conversation with my mother, I found myself talking quite casually about what I experienced all those years ago. For a long time growing up, I had some idea that the operation caused problems but I didn’t know what these were and I was not sure how my account would be received by anyone. Would my story be thought about as ‘farfetched’ or a little crazy?
We continued talking and my mother got up and walked over to a cabinet where she looked through some papers, pulling out one of my old medical reports that detailed what happened. As I read the information, my mother looked at me and said “you are a very special child”.
So, did I have an out of body experience (OBEs)?People resuscitated on the operating table speak about having an out of body experience and being drawn toward a brilliant light and while I definitely felt like I was both inside and outside of my body at the same time, I wasn’t drawn to a bright light
For centuries, people have documented “Out of Body Experiences” or Astral Projections; where the spirit is said to leave the body and float above it on another plane.
OBEs can be caused by many different things; brain trauma, sensory deprivation and simple hallucinogenic for example.
Since my brush with death at 9 years old, the subject of OBEs has continued to fascinate me and even though Science and religions may have their own explanation about where or how OBEs are created I am of the opinion that each experience is triggered by different combinations of a whole event.
Surely, this must mean that every incident is unique and is therefore a journey into the complete unknown that cannot always be explained.
Did you know that…
The term out-of-body experience was introduced in 1943 by G. N. M. Tyrrell in his book Apparitions and was adopted by researchers such as Celia Green and Robert Monroe as an alternative to belief-centric labels such as “astral projection”, “soul travel”, or “spirit walking”. OBEs can be induced by brain traumas, sensory deprivation, near-death experiences, dissociative and psychedelic drugs, dehydration, sleep, and electrical stimulation of the brain, among others. It can also be deliberately induced by some.
One in ten people have an OBE once or more commonly, several times in their life.
So, what are your views?